Febrile and First-Time Seizures
The sudden appearance of COVID-19 has created an additional challenge to the evaluation of children with "flu-like" symptoms. This article compares and contrasts influenza and coronavirus and provides a critical update on a timely topic.
AUTHOR
Cullen Clark, MD, Attending Physician, Emergency Medicine, Nationwide Children’s Hospital; Assistant Professor of Clinical Pediatrics, The Ohio State University College of Medicine, Columbus
PEER REVIEWER
Aaron Leetch, MD, FACEP, Associate Professor, Director, Combined Emergency Medicine and Pediatrics Residency, University of Arizona College of Medicine, Tucson
Executive Summary
• The American Academy of Pediatrics (AAP) defines a febrile seizure as a seizure accompanied by fever (temperature ≥ 38°C by any method) without central nervous system (CNS) infection that occurs in infants and children 6 through 60 months of age.
• A simple febrile seizure is defined as a primary generalized seizure lasting fewer than 15 minutes and without recurrence in a 24-hour period after onset.
• Febrile status epilepticus (FSE) is a febrile seizure lasting > 30 minutes or a series of seizures without return to baseline in between lasting > 30 minutes. Once again, these patients must not have a history of afebrile seizures or concerns for CNS infection to be considered FSE.
• Any febrile illness can cause a febrile seizure, but some are more associated with an increased risk of febrile seizures, particularly illnesses caused by human herpesvirus 6 (roseola), influenza, and Shigella.
• The good news is that a generally healthy, well-appearing child who has since returned to baseline after a simple febrile seizure needs no more evaluation than a history and physical exam to rule out any underlying cause of the seizure. The AAP recommends against any workup based solely on the fact the child had a febrile seizure.
• “Basic laboratory tests,” including complete blood count (CBC), serum electrolytes, calcium, magnesium, and phosphorous, are not indicated in the setting of a simple febrile seizure.
• A lumbar puncture should be strongly considered in children 6 to 12 months of age with incomplete or unknown Haemophilus influenzae type B or Streptococcus pneumoniae immunization status and a febrile seizure.
• Neuroimaging should not be performed in the routine evaluation of a child with a simple febrile seizure. Imaging should be considered only if the history or exam is concerning for trauma or obvious anatomic abnormality.
• The most recent guideline from the AAP does not recommend the use of antipyretics exclusively for the prevention of recurrent febrile seizures. Antipyretics can be recommended for fever to improve patient comfort. Since the last guidelines were published, a new study published in Pediatrics has shown the benefit of acetaminophen to prevent fever recurrence.
• The cumulative risk for recurrent febrile seizure after the first seizure is 22.7%, with no difference between boys and girls. The risk of recurrence increases with each subsequent simple febrile seizure the patient has in a lifetime: 35.6% chance of recurrence after the second febrile seizure, and 43.5% chance after the third.
Pediatric seizures are terrifying to family members and also clinicians. Fortunately, the majority of seizures do not result in serious long-term consequences. The diagnosis, evaluation, and treatment of pediatric seizures has evolved. The authors present the current best practices regarding pediatric febrile and first-time seizures.
— Ann M. Dietrich, MD, FAAP, FACEP, Editor
A seizure is defined as an abnormal, synchronous discharge of neurons in the brain resulting in a myriad of clinical manifestations. Despite being seen frequently in the emergency department (ED), these episodes can be terrifying for pediatric patients and their parents, especially if the episode is a first-time seizure. Outside the management of an actively seizing patient, there has been a lot of nuance in the evaluation and management of pediatric patients presenting after their first febrile or unprovoked seizure. Physicians in emergency medicine and pediatric emergency medicine are well versed in management of the actively seizing patient, but it is once the seizure ends and we have to determine what to do next for the patient that a lot of practice variation occurs. The goal of this review is to cover newer research and organizational guidelines regarding evaluation, management, and counseling of pediatric patients (and their parents) presenting after first-time unprovoked or febrile seizures.
Febrile Seizures
Febrile seizures can be psychologically traumatic events for patients and parents. Even though febrile seizures often are benign in nature, it is important to consider severe, underlying disease when evaluating a patient after a febrile seizure. Diagnosis and management rely on a thorough history and physical exam, which often can rule out significant acute illness or neurologic dysfunction. To begin, the definition of a febrile seizure will be reviewed.
Definition
The American Academy of Pediatrics (AAP) defines a febrile seizure as a seizure accompanied by fever (temperature ≥ 38°C by any method) without central nervous system (CNS) infection that occurs in infants and children 6 through 60 months of age.1 A simple febrile seizure is defined as a primary generalized seizure lasting less than 15 minutes and without recurrence in a 24-hour period after onset. A complex febrile seizure is defined by focality, prolonged duration (≥ 15 minutes), and recurrence in a 24-hour period after onset. Any one of these features automatically makes a febrile seizure complex. Febrile status epilepticus (FSE) is a febrile seizure lasting > 30 minutes or a series of seizures without return to baseline in between lasting > 30 minutes. Once again, these patients must not have a history of afebrile seizures or concerns for CNS infection to be considered FSE. It is difficult to distinguish FSE from CNS infection at presentation, since prolonged seizure activity in the setting of fever is highly concerning for CNS infection. Thus, FSE often is not an ED diagnosis and usually is diagnosed after CNS infection has been ruled out. Lastly, there is a newer diagnosis called generalized epilepsy with febrile seizures plus (GEFS+). This is a blanket term for several genetic disorders with febrile seizures persisting beyond 6 years of age.2 Given the rare nature and substantial differences in management, GEFS+ will not be included in this review. Table 1 presents a summary of different kinds of febrile seizures.
Epidemiology
Febrile seizure occurs in 2% to 5% of children, making it the most common cause of convulsive activity in children younger than 60 months of age.1 The incidence of febrile seizure appears to have increased slightly in the past 25 years.3 Between 25% to 30% of febrile seizures are classified as complex.4,5 A large population study in Denmark found that febrile seizures were more common in boys than girls (21% relative risk difference). The researchers also found that the highest incidence of febrile seizure was around 16 months of age and that more than 90% of children with a diagnosis of febrile seizure had their first febrile seizure before age 3 years. As many as one in 10 children with febrile seizures develop FSE, which accounts for 25% of the status epilepticus seen in children.3
Etiology/Pathophysiology
Although a febrile seizure is a well-known phenomenon, there is still much dispute about the underlying pathophysiology that causes febrile convulsions in otherwise healthy children. Any febrile illness can cause a febrile seizure, but some are more associated with increased risk of febrile seizures, particularly illnesses caused by human herpesvirus 6 (roseola), influenza, and Shigella.5 It has not been determined what is unique about these pathogens that associates them with an increased risk of febrile seizure.
Evidence points to a higher risk of febrile seizure with a higher core temperature. That being said, other predisposing factors can provoke febrile seizures at lower temperatures in children. No clinical data support the hypothesis that a rapid rise in temperature is responsible for a febrile seizure.6
Epidemiologic studies have identified a genetic predisposition for febrile seizures. Several susceptibility loci spread out over multiple chromosomes have been identified to date.7 Inheritable mutations in GABAA receptors have been found to have a temperature-dependent impairment of function that can precipitate seizures when exposed to temperatures above physiologically normal. Although febrile seizure has been identified as a major symptom in two syndromes, there still is much to be elucidated regarding specific genetic associations with febrile seizures.8
The risk of febrile seizures is known to be slightly increased for several days after certain vaccines, such as diphtheria, tetanus, and pertussis (DtaP) as well as measles mumps, and rubella (MMR) and MMR plus varicella (MMRV). An association was found between increased febrile seizure frequency and concurrent administration of inactivated influenza vaccine with either or both DtaP and pneumococcal conjugate vaccine. Although the risk was higher, the absolute risk was still small (30 febrile seizures per 100,000 patients vaccinated). The benefit of timely vaccination outweighs the slightly increased risk of febrile seizure, prompting the National Vaccine Advisory Committee to recommend not separating vaccines to different days.9
There have been numerous studies assessing the underlying factors that can lead to increased risk of febrile seizures in otherwise healthy children. Recent studies have identified a history of antenatal complications, zinc deficiency, as well as electrolyte disturbances including hyponatremia, hypomagnesemia, and hypocalcemia as risk factors that may contribute to febrile seizures.10-13
Clinical Presentation
The clinical presentations of the different types of febrile seizures are listed in Table 1. Recently, a large study group called Consequences of Prolonged Febrile Seizures (FEBSTAT) was able to identify more specific aspects of FSE to improve identification. They found FSE is more likely to be focal and convulsive in nature. FSE had a near equal distribution of presenting with one prolonged episode and presenting with multiple convulsive episodes without a return to baseline in between.14
Table 1. Types of Febrile Seizures | |||
Simple Febrile Seizure | Complex Febrile Seizure | Febrile Status Epilepticus | |
Age | 6-60 months | ||
Temperature | ≥ 38°C (100.4°F) by any method | ||
Focality | Generalized | Focal | Focal > generalized |
Duration | < 15 minutes | ≥ 15 minutes | > 30 minutes |
Recurrence | No recurrence in 24 hours | Recurrence within 24 hours of onset | Recurrence not needed for diagnosis |
Diagnostic Testing
Despite recommendations from the AAP regarding the extent of workup for children presenting with simple febrile seizure, there is still a significant amount of practice variation.15 The good news is that a generally healthy, well-appearing child who has since returned to baseline after a simple febrile seizure needs no more evaluation than a history and physical exam to rule out any underlying cause of the seizure. The AAP recommends against any workup based solely on the fact the child had a febrile seizure. Children with previous neurologic insults, known CNS abnormalities, and a history of epilepsy or nonfebrile seizures will most likely require further diagnostic evaluation.1 Further evaluation to determine the cause of the patient’s fever should be based on clinical guidelines, additional symptoms, age, and risk factors.
Laboratory Tests
Fingerstick, point-of-care blood glucose should be measured in an actively seizing patient to rule out hypoglycemia as the cause of the convulsions. It is unlikely to be helpful if the patient has returned to baseline after the seizure episode. “Basic laboratory tests,” including complete blood count (CBC), serum electrolytes, calcium, magnesium, and phosphorous, are not indicated in the setting of simple febrile seizure. Laboratory tests can be considered if the cause of fever warrants further workup but should not be obtained for the sole purpose of evaluating the cause of a simple febrile seizure.1
A retrospective review showed patients with simple febrile seizures had mild hyponatremia when compared to a control group of patients with nonfebrile seizures. This had no clinical significance because there was no relation of sodium levels to patients who were likely to have recurrent febrile seizures within 24 hours.16 Other studies identifying electrolyte disturbances as risk factors have not established whether identification or repletion of individual electrolytes would reduce the incidence of seizure. Further investigation is needed to change recommendations. As of now, there are no data to suggest screening electrolyte levels would affect ED treatment or outcomes in the setting of simple febrile seizures.11,12
Lumbar Puncture
A lumbar puncture (LP) should be performed in any patient presenting with febrile seizure and meningeal signs. Symptoms of meningitis include neck stiffness, photophobia, persistent altered mental status, petechial rash, or positive Kernig or Brudzinski sign. An LP should be strongly considered in children 6 to 12 months of age with incomplete or unknown Haemophilus influenzae type B (Hib) or Streptococcus pneumoniae (PCV) immunization status.1 By age 6 months, the patient should have received at least three doses of both Hib and PCV. Recall that children younger than 6 months of age will not qualify for the diagnosis of simple febrile seizure and, therefore, meningitis should be strongly considered as a potential source. Protective antibody levels are achieved in the vast majority of infants after two to three doses of Hib and PCV, making the likelihood of invasive infection with either bacteria highly unlikely if the patient is up to date on vaccines at age 6 months and beyond.17,18 Consider LP if the patient has a febrile seizure in the setting of pretreatment with antibiotics, since current treatment could mask the signs and symptoms of meningitis.1 The duration and type of antibiotic therapy should play into this decision, but currently there are not enough data to specify whether further workup is indicated based on the specific antibiotic or its duration of use.
No recommendations exist regarding the necessity of LP for children presenting with complex febrile seizure. A retrospective cohort review showed very little incidence of acute bacterial meningitis in children presenting with complex febrile seizure who underwent LP.4 A similar study found that there was even less likelihood of bacterial meningitis in a patient who had a subsequent febrile seizure within 24 hours (0 cases in those tested).19 Persistent altered mental status after a febrile seizure that lasts > 30 minutes is considered FSE. An LP is warranted in the initial evaluation of FSE to assess for meningitis or intracranial infection.1
Electroencephalogram
An electroencephalogram (EEG) is not indicated in a neurologically healthy child with simple febrile seizure. An EEG obtained in the ED cannot predict whether there will be a recurrence of febrile seizure or development of epilepsy.1 It is important to discuss with the child’s parents and set the expectation that an EEG would not affect the clinical outcome in the setting of simple febrile seizure.
Consider an EEG in a complex febrile seizure if there is concern for a subclinical seizure or nonconvulsive status epilepticus. A Cochrane Review found insufficient evidence to support or refute the use of EEG or the timing of obtaining an EEG after a complex febrile seizure.20 Studies included in the review indicated a tendency to have an abnormal EEG (typically generalized background slowing) if obtained within seven days of the complex febrile seizure compared to an EEG obtained more than seven days afterward. The clinical relevance of an abnormal EEG in the days after a complex febrile seizure is unknown, since many of the EEGs normalized over time.21
Neuroimaging
Neuroimaging should not be performed in the routine evaluation of a child with a simple febrile seizure.1 Imaging should be considered only if the history or exam is concerning for trauma or obvious anatomic abnormality. Similarly, for a complex febrile seizure with return to baseline, neuroimaging is unlikely to be of benefit in the ED setting unless there is concern based on exam. A study evaluating neuroimaging in the first complex febrile seizure found neither magnetic resonance imaging (MRI) nor computed tomography (CT) revealed acute intracranial pathology requiring emergent intervention in the study population.22 Another study found that, of the small number of patients that had intracranial pathology requiring emergent intervention, all had concerning physical exam findings (e.g., neurologic deficit or external signs of trauma).23 Complex febrile seizures with focality or prolonged altered mental status were more likely to be associated with abnormal findings on outpatient MRI, but these were anatomical findings that did not affect ED management.24
See Figure 1 for a summary of a typical workup indicated for febrile seizure.
Figure 1. Typical Workup for Febrile Seizures |
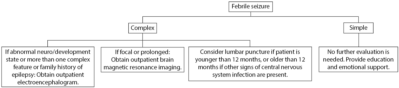 |
Adapted and reprinted from: Patel AD, Vidaurre J. Complex febrile seizures: A practical guide to evaluation and treatment. J Child Neurol 2013;28:762-767. Click the image to enlarge. |
Seizure Management
Simple Febrile Seizure
There is no good evidence to support a particular amount of time a patient should be monitored in the ED after a febrile seizure. It is advised to monitor the patient at least until they return to their neurologic baseline. If there is a protracted period of altered mental status, then pursue further workup and consider admission.26 Caregivers may express confusion and concern when little to no workup is performed in the ED before discharge. Well-worded counseling and discharge instructions are the key to easing child and caregiver anxiety while ensuring safety and understanding upon discharge. Discharge instructions should focus on routine management of febrile illness and guidance on follow-up with the patient’s pediatrician. The National Institute of Neurological Disorders and Stroke (NINDS) has an easy-to-read fact sheet designed for parents who may be concerned or need additional resources or guidance: http://bit.ly/3sWTpsQ.
The most recent guideline from the AAP does not recommend the use of antipyretics exclusively for the prevention of recurrent febrile seizures.26 Antipyretics can be recommended for fever to improve patient comfort. Since the last guidelines were published, a new study published in Pediatrics has shown the benefit of acetaminophen to prevent fever recurrence.27 The study found rectal acetaminophen (10mg/kg) every six hours for the first 24 hours after febrile seizure significantly decreased recurrence of febrile seizure during the same fever episode. It should be noted that there are no data at this time looking at the long-term effects of this intervention. This treatment course is an option for children whose anxious parents are looking for a way to prevent recurrence, but it should be used with caution, since there is a risk of acetaminophen overdose. Furthermore, if using this treatment, parents should be instructed to return to the ED if there is recurrent seizure activity.
Neither continuous nor intermittent anticonvulsant therapy is recommended to prevent recurrent simple febrile seizures.26 Although there is evidence that antiepileptic medications, such as phenobarbital, do decrease the recurrence of simple febrile seizures, the risks associated with intermittent or continuous antiepileptic therapy (e.g., allergic reactions, medication side effects) outweigh the benefit of therapy. Intermittent dosing of benzodiazepines at the onset of fever was found to reduce the occurrence of seizure. Benzodiazepines also were effective abortive medications when given at the onset of seizure activity. While beneficial in abortive management, there has been no evidence benzodiazepines alter long-term outcomes of patients with recurrent febrile seizures when compared to controls. Because of the side effects of lethargy, drowsiness, and ataxia, as well as the potential to mask another underlying cause by ceasing seizure activity, intermittent benzodiazepine therapy is not recommended for prevention or treatment of recurrent febrile seizure.26
Complex Febrile Seizure
There is no evidence to suggest treatment of complex febrile seizure should differ from the emergent management of seizure. Benzodiazepines should be the first line, followed by a second antiepileptic medication for refractory seizures. There also are no recommendations on whether to consult neurology in a patient presenting with a complex febrile seizure. When in doubt, it is always helpful to discuss concerns based on the nature of the seizure and abnormalities of the neurologic exam with a neurologist.26 There are no clear data on the efficacy of prophylactic antiepileptic therapy for complex febrile seizures. Much like with simple febrile seizures, the risks of antiepileptic drugs (AEDs) must be weighed against the benefits to determine whether medication would be appropriate for the patient. Lack of sufficient evidence for efficacy against recurrent complex febrile seizures makes initiating these medications inadvisable.5
Current studies show no benefit to workup such as EEG, neuroimaging, or LP in the immediate aftermath of a complex febrile seizure unless guided by a history and physical exam concerning for serious underlying etiology. This argues against the necessity to admit all patients with complex febrile seizures for an inpatient workup. Admission for neuromonitoring should be considered based on the patient’s clinical appearance, parental comfort, and neurology recommendations.5,19-21
Febrile Status Epilepticus
As with prolonged complex febrile seizures, the current evidence supports the notion that the presence of fever in the setting of status epilepticus should not change emergent management. The key to stopping FSE is early intervention. The longer the seizure persists, the less likely it is to resolve spontaneously. The best way to limit the delay in pharmacologic treatment of febrile or nonfebrile status epilepticus is to educate providers on identification of seizure and establish treatment protocols for ED and emergency medical services management. Given the risks associated with prolonged FSE and the numerous serious underlying etiologies, these patients tend to require admission for further workup and monitoring.28
Outcomes
Discussing outcomes with patients and their caregivers is key to counseling and setting expectations for outpatient/inpatient management.
Risk of Recurrence
The risk of febrile seizure recurrence varies significantly based on the age at which the patient had his or her first febrile seizure and the number of recurrent febrile seizures.3,26 Cumulative risk for recurrent febrile seizure after the first seizure is 22.7%, with no difference between boys and girls. The risk of recurrence increases with each subsequent simple febrile seizure the patient has in a lifetime: 35.6% chance of recurrence after the second febrile seizure and 43.5% chance after the third.3 There is a higher risk of recurrence in children whose first febrile seizure was before 12 months of age. Other risk factors for recurrence of simple febrile seizure include family history of febrile seizure, relatively low-grade fever at seizure onset, and short duration of fever before the seizure.
Risk factors that can increase the risk of recurrence after a first complex febrile seizure are similar to those of simple febrile seizures. The risk of recurrence is 15% without any of the risk factors mentioned earlier. The risk increases to 20% with one risk factor and gradually increases with each additional risk factor.5 Children presenting with FSE were at higher risk for recurrent FSE as well as febrile seizures.29
Risk of Epilepsy
The risk of epilepsy in a developmentally and neurologically normal child with simple febrile seizures is similar to that of the general population: 1%.26 The risk of epilepsy in children who have had multiple (more than four) simple febrile seizures, complex febrile seizures, onset of simple febrile seizures at an age younger than 12 months or older than 36 months, and a family history of epilepsy is slightly higher than in the general population (2.4% chance of nonfebrile seizures by age 25 years).26,30 An increase in the risk of epilepsy also was identified for patients presenting because of first-time febrile seizure with focality and/or short duration of fever prior to seizure.30 Recent studies have shown the 30-year cumulative risk of epilepsy after one febrile seizure to be 6.4%, but this was in a Danish population where the incidence of epilepsy was slightly higher than in the United States (2.2% of the general population). Additionally, the study did not distinguish between simple and complex febrile seizures. The risk of epilepsy did significantly increase with each subsequent febrile seizure.3 There have been numerous studies with a varying predicted risk of epilepsy after a complex febrile seizure. The risk may be higher after a complex febrile seizure compared to a simple febrile seizure.6,31 The risk increases if the patient exhibits more than one complex characteristic in a seizure episode.32
There are no data to suggest a simple febrile seizure causes structural brain damage or epileptogenic injury. No study has identified an intervention that reduces the risk of epilepsy in patients presenting with febrile seizures.26 The FEBSTAT study showed impaired growth of the hippocampus and hippocampal sclerosis after one year in patients who experienced FSE compared to those with simple febrile seizure. Hippocampal sclerosis is associated with temporal lobe epilepsy. While the FEBSTAT findings are suggestive, there is currently insufficient evidence to establish the risk of temporal lobe epilepsy associated with FSE.33
Risk of Neurocognitive or Psychiatric Disorder
Numerous studies have shown there is no recognizable difference in intelligence quotient, academic performance, neurocognitive inattention, behavioral abnormality, or learning between children who experienced at least one simple febrile seizure and control groups. There was a significant increase in the incidence of diagnosed psychiatric disorder in children with one or more febrile seizures, even after adjusting for epilepsy.26,34,35 The risk of lasting neurologic symptoms due to complex febrile seizure is low, but there is an increased association, since the patient is more likely to have an underlying abnormality increasing seizure risk that also could have neurocognitive effects. There is a risk of lasting neurologic deficit in FSE — as there is risk in any prolonged seizure activity.5
Risk of Death
While there is a theoretical risk of death due to aspiration, apnea, injury, or cardiac dysrhythmia associated with seizure, there are no documented cases of mortality due to simple febrile seizure.26 There was an associated 1.9% increase in mortality of patients with recurrent febrile seizures who later developed epilepsy. After adjusting for those later diagnosed with epilepsy, there was no significant increase in mortality compared to the overall population risk for children who experienced at least one febrile seizure.3
First-Time Unprovoked Seizure
When referring to first-time seizures, there are a couple of important distinctions to make: ensuring this is the first unprovoked seizure the patient is experiencing, and ruling out an obvious provoking cause, such as head trauma or CNS infection. When preparing diagnostic and treatment guidelines, the quality standards subcommittee of the American Academy of Neurology, Child Neurology Society, and American Epilepsy Society addressed several seizure morphologies limited to partial (simple and complex), partial with secondary generalization, generalized tonic-clonic, and tonic seizures. Recommendations excluded neonatal seizure (younger than 28 days of age), status epilepticus (seizure activity for more than 30 minutes), and febrile seizure.36
Epidemiology
Between 25,000 and 40,000 children per year in the United States experience a first-time unprovoked seizure.37 The prevalence of a first unprovoked seizure is less than that of febrile seizures. Approximately 0.7% of children, with a slight male predominance, will have at least one unprovoked seizure before adolescence. Children with unprovoked seizures and/or epilepsy are more likely to be of lower socioeconomic status, have increased barriers to medical care, and have preexisting developmental and/or behavioral comorbidities. There was no identified increased risk associated with a particular race or ethnic group.38,39
Etiology/Pathophysiology
The most common causes of a first-time seizure are fever, infection, and head injury.40 There are countless etiologies of abnormal, synchronized neuronal discharge presenting as seizure activity clinically. They can be divided into broad categories that allow for better characterization of the underlying cause:
- genetic;
- structural;
- metabolic;
- immune;
- infectious;
- unknown.
The history and physical exam are the keys to narrowing down the potential cause of the seizure. While identifying or narrowing the etiology may affect the workup and disposition, doing so is less likely to change the emergent management if the patient is actively seizing. If there is concern for a specific disorder, discussion with a neurologist could help guide specific diagnosis and management.40,41
Clinical Features
Seizures have countless characteristics that aid in describing the morphology and determining the type of seizure that occurred. While a seizure may be apparent if the patient arrives with an altered level of consciousness and generalized tonic-clonic activity, a first-time seizure often will resolve prior to the patient’s arrival to the ED.42 In that case, witnesses will have to explain relevant details.
A first unprovoked seizure tends to be of shorter duration than a seizure caused by known refractory epilepsy. The majority (> 90%) of first unprovoked seizures will stop spontaneously. There is an inverse relationship between the length of seizure and the likelihood it will cease without abortive medication. The longer the seizure lasts, the less likely it is to resolve spontaneously. Focal seizures tend to last longer.42
Diagnostic Studies
In the vast majority of children, the history and physical exam alone are enough to narrow down the underlying cause of a seizure. They also can identify whether a more targeted diagnostic approach with laboratory studies or neuroimaging is warranted.36 Unfortunately, there is no clinical symptom that can reliably distinguish a seizure from a nonepileptic event.
Laboratory Studies
Laboratory evaluation should be guided by the history and physical exam, not the presentation of seizure alone.36 Concerning findings on history, such as decreased intake, decreased urine output, vomiting, diarrhea, exposures, ingestions, persistent altered mental status, or specific family history, may prompt laboratory evaluation. Some possible evaluations include blood glucose concentration, electrolyte levels, liver function panel, toxicology screen, and/or markers of metabolic disturbance (e.g., lactate, ammonia, blood gas, and serum and urine ketones).36,43 Numerous studies involving adult patients have found generalized tonic-clonic seizures to be associated with elevations in creatine kinase (CK) and prolactin levels compared to psychogenic nonepileptic seizures (PNESs) previously known as pseudoseizures.44,45 Pediatric studies show a similar association, but they have been underpowered to date. It is not advised to rely solely on these laboratory markers to distinguish a seizure from other nonepileptic episodes in children.46,47 It should be noted that other seizures, such as partial and absence seizures, are less likely to have associated elevations in CK.45
Lumbar Puncture
Insufficient evidence exists to recommend LP for the evaluation of first-time unprovoked seizure.36 If meningeal signs are present, or a high suspicion exists for CNS infection, perform an LP in the ED. If there is concern for elevated intracranial pressure, obtain a CT of the head to assess for signs of impending herniation prior to LP. The likelihood of an isolated, first-time seizure being the presenting sign of meningoencephalitis is low. In patients presenting with a first-time seizure with status epilepticus, less than 1% were found to have bacterial meningitis, and 1.8% had viral encephalitis. Of the patients who had meningitis or encephalitis, most presented with fever and status epilepticus.48
EEG
EEG was found to be helpful in predicting the risk of recurrence of seizure after a first seizure. EEG interpretation in the ED was difficult due to postictal slowing, making prognosis much less accurate. It is recommended that an EEG be part of the evaluation of a patient with a first-time unprovoked seizure, but it should not routinely be performed in the ED. There is still debate over the optimal timing of the EEG, given the higher likelihood of abnormalities in the first 24-48 hours after a seizure, which may not be useful diagnostically.36,41
Neuroimaging
Neuroimaging is not indicated solely for presentation of a first unprovoked seizure.36 Children with generalized onset seizures with normal neurodevelopmental history and normal neurologic exam do not require emergent imaging unless there is clinical suspicion for an intracranial abnormality, such as intracranial mass, bleeding, or structural abnormality.41 Emergent neuroimaging is indicated if there is a persistent or postictal deficit, or if the child has not returned to baseline after 30 minutes from the onset of seizure.
MRI is more sensitive than a CT scan for intracranial abnormalities in patients presenting with first-time unprovoked seizure. MRI should be considered if there is significant cognitive or motor impairment, abnormal neurologic exam, a partial seizure without generalization, or an abnormal EEG in a child younger than 1 year of age.36 In a single-center, cross-sectional study, of the 13 patients who had clinically significant findings on neuroimaging, only one had an abnormality seen on MRI and not CT. Every other patient’s clinically significant intracranial abnormality was seen on CT.
Studies show anywhere from 4% to 11% of children presenting after an unprovoked first seizure with persistent neurologic deficit had clinically significant findings on neuroimaging that affected their overall treatment course. Hemorrhage and infarction were the most common abnormalities identified. Children younger than 18 months of age, those with high-risk medical histories (e.g., neoplasm, shunt, cardiac defect, sickle cell disease, etc.), and those with persistent Todd’s paralysis were at higher risk for urgent intracranial pathology requiring intervention.49-5 1 Less than 1% of the children with an identified intracranial abnormality required emergent intervention that changed their ED course.51
Differential Diagnosis
The differential diagnosis is wide. Rather than run through the extensive list of possible mimics or underlying causes, this article will focus on the more common diagnoses that present with seizure-like symptoms or episodes that do not represent actual seizures. It is important to note that there are a couple of “can’t miss” diagnoses when assessing a child with a suspected seizure. Cardiac dysrhythmias (e.g., prolonged QT syndromes, supraventricular tachycardia, ventricular tachycardia, etc.) and cerebrovascular accident must be considered and evaluated based on suspicion, since a delayed diagnosis can lead to severe morbidity and mortality.41
PNESs are relatively rare in the pediatric population compared to adults. Be wary; up to one-third of PNESs can occur in patients with epilepsy. PNESs typically are brought on by emotional stress. While the seizures are psychogenic, they typically are not volitionally caused by the patient. PNES is very responsive to appropriate treatment.40
Management
Like febrile seizures, there is no evidence to suggest that treatment of a first-time, unprovoked seizure should differ from the emergent management of seizure. There also is no good evidence to support a particular amount of time a patient should be monitored in the ED after a first unprovoked seizure. It is advised to monitor the patient at least until they return to their neurologic baseline. If there is a protracted period of altered mental status, then pursue further workup and consider admission. There are no guidelines or recommendations regarding the management of absence and atonic seizures outside of the acute setting, since these events typically are harder to recognize initially and usually several episodes have occurred prior to identification and medical attention.37
Seizure Prophylaxis
Prophylactic AEDs are not typically indicated after the first unprovoked seizure unless there are factors suggesting a strong possibility of recurrence or identification of a specific syndrome or etiology.37,41 Studies have found that treatment with antiepileptic medications can reduce the rate of seizure recurrence.52,53 More recent adult literature points to an improvement in quality of life with the immediate initiation of antiepileptic therapy in those at higher risk of recurrence compared to delayed therapy initiation.54 There is no such study exclusive to pediatrics, but a follow-up to the University of Cambridge’s Medical Research Council Multicentre trial for Early Epilepsy and Single Seizures (commonly called MESS) study identified a reduction of seizure recurrence with early AED therapy in a population including both adult and pediatric patients. It found no significant improvement in quality of life in that patient population.55
The reason for the hesitance in initiating prophylactic AEDs after a first unprovoked seizure in pediatrics is the concern for side effects. Antiepileptic drugs have numerous known side effects in children. Side effects most commonly include somnolence and behavioral disturbances, such as anxiety, attention issues, and mood disturbances. These studies include historically used medications (valproate, phenytoin, and phenobarbital) as well as newer medications (levetiracetam, lamotrigine, topiramate, and oxcarbazepine).56-58 There were some differences in additional side effects between individual medications, but the issues with somnolence and behavioral changes are ubiquitous.56 There has been attention on the effects of AEDs on behavioral and cognitive abilities in children for a long time.59 While evidence thus far has indicated a relationship, there is further study looking into the effects of long-term neurocognitive effects of AED treatment during early childhood. Evidence supports a decline in neurocognitive function in animal models seen with early childhood AED exposure. Similarities are present thus far in limited human studies.60,61 Further studies are required to determine if the risk associated with AEDs is worth the benefit of the potential reduction in recurrence and long-term development of epilepsy. AEDs should not routinely be initiated from the ED in a patient presenting with a first-time unprovoked seizure, especially without consultation of a pediatric neurologist.37,41
Disposition
There are no current recommendations or guidelines regarding disposition of pediatric patients presenting with first-time, unprovoked seizures, who have returned to their neurologic baseline and do not have evidence of underlying significant disease. It is implied that these patients are candidates for discharge from the ED with close follow-up for outpatient workup as long as the caregivers and consultants are in agreement. If there is concern about a patient who potentially can be discharged, discussion with a pediatric neurologist can help determine aspects of the history or physical exam that require further workup. Furthermore, consultation with a pediatric neurologist can aid in arranging close follow-up for the patient.37
Risk of Seizure Recurrence
Good counseling on the risk of recurrence is helpful to the patient and family in easing uncertainty and managing expectations. Without a discernible cause of the first-time seizure, the rate of recurrence is around 50% in the first two years.37,62,63 Recurrence was most likely to occur within two years of the first seizure.63 Recent prospective studies indicate the risk may be higher, but there is still a wide range of estimated risk of recurrence.64,65 The caregivers should be advised to return to the ED if another seizure occurs, since it may change the management from outpatient to inpatient.
Seizure Precautions
Seizures can put a child at risk for one or more injuries given the environment they are in at the time of the seizure. All families and caregivers of patients presenting after seizures should receive information on seizure precautions and seizure first aid. There are several resources providing extensive seizure precautions for pediatric patients. Some of the recommended websites are:
- HealthyChildren.org: http://bit.ly/3orIMek
- The Epilepsy Foundation: http://bit.ly/36gEcJn
- KidsHealth.org: http://bit.ly/39l7o48
Summary
Seizures in pediatric patients are terrifying events for them and their caregivers. The majority of these events are benign in nature and do not lead to serious adverse outcomes. There has been a lot of practice variation regarding the diagnosis and management of febrile and first-time unprovoked seizures over the years, despite guidelines from professional organizations. Laboratory evaluation, neuroimaging, electroencephalogram, and lumbar puncture often are not indicated in most of these patients unless a specific concern arises from aspects of their history and physical exam. Often, if the patient has returned to his or her normal state of health after the seizure, the patient can be discharged for completion of the workup as an outpatient. Patients typically do not require antiepileptic medications at the time of discharge. It is important to discuss the patient’s case with a pediatric neurologist if any concerns about serious underlying disease or diagnostic uncertainty are present. This is to ensure the ED workup has been adequate and the patient can have close follow-up arranged. Counseling patients and their caregivers is of the utmost importance in ensuring they understand the necessity of follow-up and seizure precautions for home. Discussing risk of recurrence and outcomes can significantly reduce caregiver anxiety and improve patient safety.
References
- American Academy of Pediatrics Subcommittee on Febrile Seizures. Febrile seizures: Guideline for the neurodiagnostic evaluation of the child with simple febrile seizure. Pediatrics 2011;127:389-394.
- Panayiotopoulos CP. Generalized epilepsies with febrile seizures plus (GEFS; autosomal dominant epilepsy with febrile seizures plus). Epilepsy Foundation. Updated May 31, 2008. https://www.epilepsy.com/livin...
- Dreier JW, Li J, Sun Y, Christensen J. Evaluation of long-term risk of epilepsy, psychiatric disorders, and mortality among children with recurrent febrile seizures, a national cohort study in Denmark. JAMA Pediatr 2019;173:1164-1170.
- Kimia A, Ben-Joseph EP, Rudloe T, et al. Yield of lumbar puncture among children who present with their first complex febrile seizure. Pediatrics 2010;126:62-69.
- Whelan H, Harmelink M, Chou E, et al. Complex febrile seizures — A systematic review. Dis Mon 2017;63:5-23.
- Berg AT. Are febrile seizures provoked by a rapid rise in temperature? Am J Dis Child 1993;147:1101-1103.
- Ellenberg JH, Nelson KB. Febrile seizures and later intellectual performance. Arch Neurol 1978;35:17-21.
- Kang J-Q, Shen W, Macdonald RL. Why does fever trigger febrile seizures? GABAA receptor gamma2 subunit mutations associated with idiopathic generalized epilepsies have temperature-dependent trafficking deficiencies. J Neurosci 2006;26:2590-2597.
- Duffy J, Weintraub E, Hambidge SJ, et al. Febrile seizure risk after vaccination in children 6 to 23 months. Pediatrics 2016;138:e20160320.
- Baek S-J, Byeon JH, Eun S-H, et al. Risk of low serum levels of ionized magnesium in children with febrile seizure. BMC Pediatr 2018;18:297.
- Sharawat IK, Singh J, Dawman L, Singh A. Evaluation of risk factors associated with first episode febrile seizure. J Clin Diagn Res 2016;10:SC10-SC13.
- Yousefichaijan P, Eghbali A, Rafeie M, et al. The relationship between iron deficiency anemia and simple febrile convulsion in children. J Pediatr Neurosci 2014;9:110-114.
- Ganesh R, Janakiraman L. Serum zinc levels in children with simple febrile seizure. Clin Pediatr (Phila) 2008;47:164-166.
- Shinnar S, Hesdorffer DC, Nordli DR Jr, et al. Phenomenology of prolonged febrile seizures: Results of the FEBSTAT study. Neurology 2008;71:170-176.
- Hampers LC, Thompson DA, Bajaj L, et al. Febrile seizure: Measuring adherence to AAP guidelines among community ED physicians. Pediatr Emerg Care 2006;22:465-469.
- Thoman JE, Duffner PK, Shucard JL. Do serum sodium levels predict febrile seizure recurrence within 24 hours? Pediatr Neurol 2004;31:342-344.
- Centers for Disease Control and Prevention. About Hib vaccines. Updated Feb. 13, 2018. https://www.cdc.gov/vaccines/v...
- Centers for Disease Control and Prevention. About pneumococcal vaccines. Updated Dec. 6, 2017. https://www.cdc.gov/vaccines/v...
- Fletcher EM, Sharieff G. Necessity of lumbar puncture in patients presenting with new onset complex febrile seizures. West J Emerg Med 2013;14:206-211.
- Shah PB, James S, Elayaraja S. EEG for children with complex febrile seizures. Cochrane Database Syst Rev 2017;2017:CD009196.
- Joshi C, Wawrykow T, Patrick J, Prasad A. Do clinical variables predict an abnormal EEG in patients with complex febrile seizures? Seizure 2005;14:429-434.
- Teng D, Dayan P, Tyler S, et al. Risk of intracranial pathologic conditions requiring emergency intervention after a first complex febrile seizure episode among children. Pediatrics 2006;117:304-308.
- Kimia AA, Ben-Joseph E, Prabhu S, et al. Yield of emergent neuroimaging among children presenting with a first complex febrile seizure. Pediatr Emerg Care 2012;28:316-321.
- Hesdorffer DC, Chan S, Tian H, et al. Are MRI-detected brain abnormalities associated with febrile seizure type? Epilepsia 2008;49:765-771.
- Patel AD, Vidaurre J. Complex febrile seizures: A practical guide to evaluation and treatment. J Child Neurol 2013;28:762-767.
- Steering Committee on Quality Improvement and Management, Subcommittee on Febrile Seizures American Academy of Pediatrics. Febrile seizures: Clinical practice guideline for the long-term management of the child with simple febrile seizures. Pediatrics 2008;121:1281-1286.
- Murata S, Okasura K, Tanabe T, et al. Acetaminophen and febrile seizure recurrences during the same fever episode. Pediatrics 2018;142:e20181009.
- Seinfeld S, Shinnar S, Sun S, et al. Emergency management of febrile status epilepticus: Results of the FEBSTAT study. Epilepsia 2014;55:388-395.
- Hesdorffer DC, Shinnar S, Lax DN, et al. Risk factors for subsequent febrile seizures in the FEBSTAT study. Epilepsia 2016;57:1042-1047.
- Pavlidou E, Panteliadis C. Prognostic factors for subsequent epilepsy in children with febrile seizures. Epilepsia 2013;54:2101-2107.
- Annegers JF, Hauser WA, Shirts SB, Kurland LT. Factors prognostic of unprovoked seizures after febrile convulsions. N Engl J Med 1987;316:493-498.
- Abou-Khalil B, Andermann E, Andermann F, et al. Temporal lobe epilepsy after prolonged febrile convulsions: Excellent outcome after surgical treatment. Epilepsia 1993;34:878-883.
- Lewis DV, Shinnar S, Hesdorffer DC, et al. Hippocampal sclerosis after febrile status epilepticus: The FEBSTAT study. Ann Neurol 2014;75:178-185.
- Ellenberg JH, Nelson KB. Febrile seizures and later intellectual performance. Arch Neurol 1978;35:17-21.
- Verity CM, Greenwood R, Golding J. Long-term intellectual and behavioral outcomes of children with febrile convulsions. N Engl J Med 1998;338:1723-1728.
- Hirtz D, Ashwal S, Berg A, et al. Practice parameter: Evaluating a first nonfebrile seizure in children: Report of the quality standards subcommittee of the American Academy of Neurology, The Child Neurology Society, and The American Epilepsy Society. Neurology 2000;55:616-623.
- Hirtz D, Berg A, Bettis D, et al. Practice parameter: Treatment of the child with a first unprovoked seizure: Report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 2003;60:166-175.
- Cui W, Kobau R, Zack MM, et al. Seizures in children and adolescents aged 6-17 years - United States, 2010-2014. MMWR Morb Mortal Wkly Rep 2015;64:1209-1214.
- Russ SA, Larson K, Halfon N. A national profile of childhood epilepsy and seizure disorder. Pediatrics 2012;129:256-264.
- Sidhu R, Velayudam K, Barnes G. Pediatric seizures. Pediatr Rev 2013;34:333-341;342.
- Fine A, Wirrell EC. Seizures in children. Pediatr Rev 2020;41:321-347.
- Shinnar S, Berg AT, Moshe SL, Shinnar R. How long do new-onset seizures in children last? Ann Neurol 2001;49:659-664.
- Guerrero RB, Salazar D, Tanpaiboon P. Laboratory diagnostic approaches in metabolic disorders. Ann Transl Med 2018;6:470.
- Javali M, Acharya P, Shah S, et al. Role of biomarkers in differentiating new-onset seizures from psychogenic nonepileptic seizures. J Neurosci Rural Pract 2017;8:581-584.
- Nass RD, Sassen R, Elger CE, Surges R. The role of postictal laboratory blood analyses in the diagnosis and prognosis of seizures. Seizure 2017;47:51-65.
- Mahmoud AT, El Daghady AAM. Serum prolactin and creatine kinase levels in epileptic and non-epileptic seizures. Alexandria Journal of Pediatrics 2005;19:217-222.
- Lahat E, Eshel G, Heyman E, et al. Elevated serum creatine kinase. Following febrile seizures. Clin Pediatr (Phila) 1989;28:449-451.
- Michelson KA, Lyons TW, Johnson KB, et al. Utility of lumbar puncture in children presenting with status epilepticus. Pediatr Emerg Care 2017;33:544-547.
- Aprahamian N, Harper MB, Prabhu SP, et al. Pediatric first time non-febrile seizure with focal manifestations: Is emergent imaging indicated? Seizure 2014;23:740-745.
- Sharma S, Riviello JJ, Harper MB, Baskin MN. The role of emergent neuroimaging in children with new-onset afebrile seizures. Pediatrics 2003;111:1-5.
- Dayan PS, Lillis K, Bennett J, et al. Prevalence of and risk factors for intracranial abnormalities in unprovoked seizures. Pediatrics 2015;136:e351-e360.
- [No authors listed.] Randomized clinical trial on the efficacy of antiepileptic drugs in reducing the risk of relapse after a first unprovoked tonic-clonic seizure. First Seizure Trial Group (FIR.S.T. Group). Neurology 1993;43:478-483.
- Marson A, Jacoby A, Johnson A, et al. Immediate versus deferred antiepileptic drug treatment for early epilepsy and single seizures: A randomised controlled trial. Lancet 2005;365:2007-2013.
- Bao EL, Chao LY, Ni P, et al. Antiepileptic drug treatment after an unprovoked first seizure: A decision analysis. Neurology 2018;91:e1429-e1439.
- Jacoby A, Gamble C, Doughty J, et al. Quality of life outcomes of immediate or delayed treatment of early epilepsy and single seizures. Neurology 2007;68:1188-1196.
- Bath KG, Scharfman HE. Impact of early life exposure to antiepileptic drugs on neurobehavioral outcomes based on laboratory animal and clinical research. Epilepsy Behav 2013;26:427-439.
- Nevitt SJ, Sudell M, Weston J, et al. Antiepileptic drug monotherapy for epilepsy: A network meta-analysis of individual participant data. Cochrane Database Syst Rev 2017;12:CD011412.
- Anderson M, Egunsola O, Cherrill J, et al. A prospective study of adverse drug reactions to antiepileptic drugs in children. BMJ Open 2015;5:e008298.
- Behavioral and cognitive effects of anticonvulsant therapy. American Academy of Pediatrics Committee on Drugs. Pediatrics 1995;96:538-540.
- Palac S, Meador KJ. Antiepileptic drugs and neurodevelopment: An update. Curr Neurol Neurosci Rep 2011;11:423-427.
- Gedzelman ER, Meador KJ. Neurological and psychiatric sequelae of developmental exposure to antiepileptic drugs. Front Neurol 2012;3:182.
- Berg AT. Risk of recurrence after a first unprovoked seizure. Epilepsia 2008;9(Suppl 1):13-18.
- Mizorogi S, Kanemura H, Sano F, et al. Risk factors for seizure recurrence in children after first unprovoked seizure. Pediatr Int 2015;57:665-669.
- Ramos-Lizana J, Aguirre-Rodríguez J, Aguilera-López P, Cassinello-García E. Recurrence risk after a first remote symptomatic unprovoked seizure in childhood: A prospective study. Dev Med Child Neurol 2009;51:68-73.
- Sartori S, Nosadini M, Tessarin G, et al. First-ever convulsive seizures in children presenting to the emergency department: Risk factors for seizure recurrence and diagnosis of epilepsy. Dev Med Child Neurol 2019;61:82-90.
